Revenue cycle management in healthcare is often mistaken for the medical billing and coding functions within a medical practice or larger healthcare organization. Revenue Cycle Management (RCM) is more than just billing and collections. It begins with the first patient contact and ends with a response to an online review. Here is a comprehensive 2025 Guide to Revenue Cycle Management.
RCM is a vital part of healthcare and is in direct correlation with the financial prosperity of any healthcare organization. This article will explain what RCM is, why it is essential, and what your healthcare organization can do to improve this essential element within the organization.
Table of Contents
Take a little break, grab a beverage, and watch our video below, explaining the differences between billing and RCM. If time is not on your side today, simply scroll down past the video.

What is Revenue Cycle Management in Healthcare?
The Revenue Cycle Management process in healthcare manages the financial aspects of healthcare. It begins with patient registration and ends when payment is collected. It may even involve activities beyond collection. RCM plays a crucial role in the financial well-being of healthcare organizations as it determines the accuracy and efficiency of reimbursements for services rendered.
RCM within healthcare can be broken up into 13 steps or processes that make up the healthcare revenue cycle. Below is a summary of the 13 steps of revenue cycle management.
1. Patient Pre-registration: Collects crucial patient information before care encounters for accurate billing and financial transactions.
2. Appointment Scheduling: Streamlines patient schedules for optimal resource use, reducing no-shows and contributing to financial health.
3. Insurance Verification: Confirms patient’s insurance coverage and benefits pre-service, setting the stage for accurate billing and revenue flow.
4. Point-of-Service Collections: Involves collecting co-pays and balances during the visit, enhancing accounts receivable management in a timely manner.
5. Charge Capture: Ensures accurate recording of billable services, crucial for efficient claims processing and revenue optimization.
6. Coding and Documentation: Translates medical services into standardized codes, essential for efficient claim submission and reducing denials.
7. Claim Submission: Timely submission to payors accelerates reimbursement, minimizing revenue leakage and ensuring financial health.
8. Claim Rejections and Denials Management: Proactively addresses issues to ensure optimal revenue recovery and financial stability.
9. Payment Posting: Essential for maintaining up-to-date financial records, contributing to efficient accounts receivable management.
10. Patient Statements and Follow-Up: Vital for patient care and financial stability, ensuring clear communication on outstanding balances and collecting payments.
11. Denials Analysis and Appeals: Identifies patterns, contributing to efficient claims processing and minimizing revenue loss.
12. Compliance and Auditing: Imperative for maintaining industry standards, ensuring adherence to regulations, and identifying areas for enhancement.
13. Financial Reporting and Analysis: Provides insights into revenue trends, supporting informed decisions for continuous improvement in revenue cycle management.
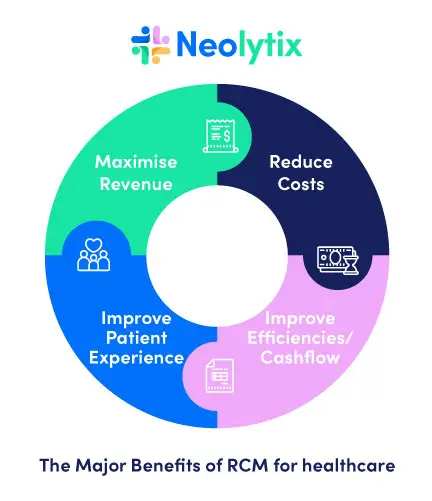
The goal of RCM is two-fold. Firstly, it ensures that healthcare providers receive accurate and timely payment for the services they provide. Secondly, if done correctly, it provides patients with a positive experience. The diagram below shows the correlated benefits of a well optimized revenue cycle.
Why is RCM important to Healthcare Organizations?
For many healthcare organizations, certain operations, or clusters of them, are managed in isolation. For instance, the front end of the billing cycle and the back end are managed by separate managers, with no overarching governing entity in place.
In this instance, each department fends for themselves and tries to do everything correctly that they are supposed to, but they also miss out on mutual beneficial opportunities or cases to create an interdepartmental synergy.
Inefficient or bad practices within certain processes can stay unnoticed for long periods. One reason could be due to staff being too busy and lacking the resources to look into and report on the same inefficiencies that keep happening. In addition, as mentioned before, the silo effect within certain departments and the lack of overarching accountability can hinder the discovery of such efficiencies.
But if RCM is managed from a holistic approach, many benefits can come to fruition that wouldn’t have been the case in an “everybody for themselves” scenario. Here are some of the most common benefits healthcare organizations with stern RCM structures experience:
- Financial stability:
RCM assists healthcare organizations with efficient financial management. It also ensures they receive reimbursement for services in a timely, accurate way. This contributes to the financial stability of the organization.
- Improved patient experience:
RCM streamlines the billing and payment process. This reduces confusion and frustration for patients. It leads to a better overall experience.
- Compliance with regulations:
RCM helps healthcare organizations comply with billing and reimbursement regulations, such as the Affordable Care Act and HIPAA.
- Better Data management:
RCM helps healthcare organizations to collect, store, and analyze data related to patient care, treatment, and billing. This information can be used to improve patient care and make informed decisions.
- Increased revenue:
By improving the efficiency and accuracy of the billing and payment process, RCM can increase revenue for healthcare organizations. This can help them to continue providing quality care to their patients.
Get Faster Reimbursements at Reduced Rates
let us handle your Revenue cycle management. get paid faster and easier
Contact Us Today!
How can healthcare organizations improve RCM?
Continued enhancement of Revenue Cycle Management (RCM) is imperative for the sustained success of healthcare organizations. Here are detailed strategies to fortify and refine RCM processes:
Utilize Advanced Medical Billing Software:
Integrate state-of-the-art billing software designed to streamline processes, minimize errors, and improve overall accuracy in billing and coding. Robotic Process Automation (RPA) entails the automation of rule-based processes and is becoming more prevalent withing many steps of RCM.
Invest in Staff Training:
Training in coding and compliance updates is often neglected as staff are overworked and don’t have the capacity to do research and stay up to date with changes. Prioritize ongoing training programs for staff, ensuring they stay abreast of the latest developments and best practices in billing and coding procedures.
Enhance Patient Education:
Develop comprehensive educational initiatives for patients, emphasizing the significance of providing accurate information and ensuring prompt payments to facilitate smoother and more efficient processes.
Apart from ensuring efficiency, patient education can help manage expectations, which in turn leads to an improved patient experience. A better patient experience, on the other hand, leads to an improved reputation of the healthcare organization.
Regular Audits for Compliance:
Conduct routine audits to meticulously assess and uphold compliance with the ever-evolving industry regulations and standards, proactively identifying and addressing any potential issues.
Coding audits help mitigate revenue losses and improve compliance, yet organizations often go years without doing it. When organizations can’t do this vital exercise themselves, it is advised that they outsource this function at least once a year.
Billing support companies, like Neolytix, provide thorough coding audits and improvement services. This assists in enhancing accuracy, documentation, revenue, coding risk management, and compliance.
Implement Data Analytics:
Harness the power of data analytics tools to gain profound insights into revenue trends, enabling data-driven decision-making and strategic planning for continuous improvement.
Analytical data from the revenue cycle can reveal opportunities for resource optimization, cost-cutting initiatives, automation possibilities, etc.
Optimize Appointment Scheduling:
Deploy advanced scheduling systems to optimize appointment planning, reduce no-show rates, and maximize the efficient use of resources within the healthcare facility.
Within larger healthcare organizations, patient access is becoming a focus point of the revenue cycle and ground zero of the patient experience. Patient Access Services offer hospitals, ambulatory care centers, physician groups, clinics, and similar entities a platform to enhance revenue, efficiency, and patient experience from the outset of the revenue cycle.
Proactive Denials Management:
Establish a proactive denials management system, focusing on swift identification and resolution of claim rejections and denials to minimize financial losses and maintain optimal revenue recovery.
In addition to managing denials with payors, healthcare organizations should also step back and ask: ‘Are we getting the reimbursements we deserve?’
Rajat Bhatnagar from Neolytix once stated: “Most Payers will offer you the bottom-of-the-barrel prices for services.” This might be a slight exaggeration, but it wouldn’t hurt to try and negotiate a better contract through payor contract negotiations.
Streamlined Communication:
Foster enhanced communication channels between billing departments, insurance companies, and patients, promoting transparency and clarity in information exchange to prevent misunderstandings and delays.
Communication issues are usually rife within silos, and it’s one of the critical areas that RCM addresses to ignite synergy within the system.
Embrace Telehealth Technologies:
Integrate innovative telehealth technologies into the RCM framework, facilitating remote patient monitoring (RPM), streamlined billing processes, and seamless exchange of critical healthcare information.
Remote Patient Monitoring has been growing phenomenally since the Covid-19 Pandemic spurred it on. It is predicted that the RPM market will continue to grow by a compound annual growth rate (CAGR) of 18.6% from 2024 to 2030.
Slotting RPM into your service offering not only improves patient outcomes and the patient experience but also injects additional reimbursement revenue into the revenue cycle.
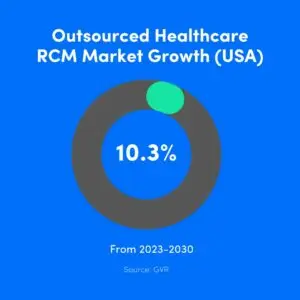
Outsource RCM Services:
Consider the strategic outsourcing of RCM services to specialized agencies equipped with expertise in the field. This can bring efficiency, proficiency, and a fresh perspective to the revenue cycle processes.
Apart from their expertise throughout the entire RCM spectrum, the objective insights from outsourced RCM providers like Neolytix, give the decision-makers within the healthcare organizations something concrete to work with, empower them with objective accurate data to make strategically correct data-driven decisions.
What does the future hold for RCM?
If you’re here to explore where you can improve Revenue Cycle Management, but discovered throughout this article that your organization is ticking all the boxes, then the next section is for you.
As healthcare and technology continue to intertwine, the future of RCM holds exciting prospects for increased efficiency, transparency, and patient-centricity, positioning it as a crucial component in the evolving landscape of healthcare administration.
Below, you will find highlights of the expected evolution of RCM for 2024.
Integration of Artificial Intelligence (AI) and Machine Learning (ML)
Anticipate the integration of AI and ML algorithms into RCM processes for enhanced predictive analytics, fraud detection, and automation of routine tasks, fostering increased efficiency and accuracy.
A good example of AI integration is within Patient Access. Neolytix, for instance, offers omnichannel communication capabilities to their Patient Access teams. Patients can use their preferred channels to contact the organization.
In the back-end, all calls are transcribed, and every form of communication is then analyzed by AI to determine the patient analysis. This information is then used to assist in improving future communications to create a better patient experience.
Expansion of Telehealth and Remote Services
We have already elaborated on the future of RPM mentioned and that the market will continue to grow at 18.6% for the next six years.
With the continued growth of telehealth, RCM will see further integration of remote patient monitoring, virtual consultations, and digital billing solutions, emphasizing the importance of adaptable and comprehensive RCM frameworks.
Focus on Consumer-Centric RCM:
Future RCM strategies will increasingly prioritize a consumer-centric approach, offering patients more control and visibility into their financial responsibilities, billing processes, and payment options through user-friendly interfaces.
Patient Access teams would need to be integrated with new developments in consumer centric RCM to provide a seamless experience for the patient.
Predictive Analytics for Financial Planning:
RCM will leverage advanced predictive analytics to foresee revenue trends, optimize financial planning, and proactively address potential challenges, contributing to the overall financial health of healthcare organizations.
This will also pave the way for automation opportunities in the form of robotic process automation with the aim of reducing errors and costs over the long term.
Regulatory Compliance and Evolving Reimbursement Models:
RCM will continually adapt to evolving regulatory requirements and changes in reimbursement models, necessitating agile and flexible systems that can promptly adjust to shifting healthcare policies.
Being proactive requires extensive knowledge of changes within the industry and events taking shape on the horizon. With most healthcare organizations focusing on short-term operational requirements and making ends meet, they might be slow at adapting to these changes.
The Impact of Technology on Revenue Cycle Management in Healthcare
Revenue cycle management in healthcare is undergoing a transformative shift due to advancements in technology. Healthcare revenue cycle management solutions are increasingly leveraging Artificial Intelligence (AI), Machine Learning (ML), and Robotic Process Automation (RPA) to optimize processes, reduce errors, and enhance efficiency. For instance, AI-powered analytics provide deeper insights into revenue trends, helping organizations make data-driven decisions that improve their hospital revenue cycle management.
Additionally, telehealth technologies and remote patient monitoring (RPM) are becoming integral components of the healthcare revenue cycle definition. These innovations not only improve patient access and care but also streamline billing processes, making the revenue cycle workflow more efficient. By embracing these best practices in revenue cycle management, healthcare providers can ensure a smoother, more accurate revenue cycle management process.
This integration of technology is redefining the revenue cycle in healthcare, making it more adaptable and patient-centric.
Take a Short-Cut to RCM Efficiency
The fastest way to improve efficiency throughout the revenue cycle is to call in the experts. Neolytix has been helping healthcare organizations nationwide improve revenue, cut down on costs, and improve the patient experience for over 13 years.
Revolutionize your Revenue Cycle Management (RCM) with our industry-best blueprint. Whether you’re starting up, optimizing, or scaling, our stand-alone RCM Consulting services offer transformative solutions.
Increase revenue and reduce costs through Revenue Leakage Analysis, error trend detection, and expedited insurance reimbursements. Our integrated approach ensures governance and transparency across the entire cycle, from patient contact to reconciliation.
Neolytix enables holistic analysis, fostering cross-departmental synergy and empowering your organization with Revenue Intelligence through tailored metrics and in-depth reporting for proactive improvement strategies.
Schedule a demo with an RCM expert and see how Neolytix can improve your revenue cycle.
Essential FAQs for Healthcare Revenue Cycle Management
Revenue cycle management (RCM) in healthcare is the process of managing the financial aspects of patient care, from registration and appointment scheduling to billing and payment collection. It ensures that healthcare providers receive timely and accurate payments for their services, ultimately supporting the financial health of the organization. Revenue cycle management healthcare involves various stages, including patient pre-registration, insurance verification, and payment posting.
Revenue cycle management is essential in healthcare because it directly impacts the financial stability of healthcare organizations. Efficient RCM healthcare processes help ensure timely reimbursements, improve cash flow, and enhance overall financial performance.
The importance of revenue cycle management in healthcare cannot be overstated, as it supports both the financial health of the organization and the quality of patient care.
The phases of revenue cycle management in healthcare include patient pre-registration, insurance verification, charge capture, coding and documentation, claim submission, payment posting, and financial reporting. Each phase is crucial for ensuring accurate billing and efficient reimbursement. Understanding these components of revenue cycle management is key to define RCM and optimizing the entire hospital revenue cycle process.
Scrubbers are automated tools used in the revenue cycle management process to identify and correct errors in medical claims before submission. They help reduce claim denials and improve the accuracy of billing, ensuring a smoother revenue cycle in healthcare.
By using scrubbers, hospital RCM services can enhance their efficiency and accuracy.
Finance plays a critical role in healthcare revenue cycle management by overseeing the entire revenue cycle workflow, ensuring accurate billing, and managing cash flow. Effective financial management in RCM helps healthcare organizations maintain financial stability and continue providing quality patient care.
Revenue cycle management meaning in healthcare encompasses all the administrative and clinical functions that contribute to capturing, managing, and collecting patient service revenue. Understanding RMC’s role in optimizing financial outcomes and improving operational efficiency within healthcare organizations is paramount when you define revenue cycle management.
Hospital RCM services provide specialized support in managing the revenue cycle, from patient intake to final payment. These services help hospitals reduce administrative burdens, improve billing accuracy, and ensure compliance with regulations. By outsourcing revenue cycle management services, healthcare organizations can focus more on patient care while maintaining financial health.
Healthcare revenue cycle solutions are comprehensive systems and tools designed to manage and optimize the financial processes within a healthcare organization. These solutions include advanced billing software, data analytics, and automated tools like scrubbers. Implementing these solutions enhances the overall efficiency of the revenue cycle for healthcare.
RCM in healthcare refers to the processes and strategies used to manage the financial aspects of patient care. It is important because it ensures that healthcare providers are reimbursed accurately and promptly for their services. Understanding what RCM is in healthcare helps organizations implement effective practices to optimize their revenue cycles.
Understanding revenue cycle management in healthcare enables organizations to streamline their financial processes, reduce administrative burdens, and enhance cash flow. By grasping the intricacies of what is healthcare revenue cycle management, healthcare providers can implement strategies that ensure timely reimbursements and improved patient satisfaction. This knowledge also helps in identifying and rectifying inefficiencies within the revenue cycle management hospital framework.
A clear revenue cycle definition in healthcare helps providers outline the specific processes and components involved in managing their financial operations. This clarity aids in implementing targeted improvements, such as advanced billing software and proactive denials management. A well-defined revenue cycle management process contributes to better financial health and operational efficiency, making it a cornerstone of successful healthcare RCM strategies.
Schedule a Free Consultation to learn more about optimizing your revenue cycle
Complete the form and someone from our team will be in touch with you!



