Table of Contents
1. What is AR in Healthcare Billing?
Accounts Receivable (AR) is a critical component representing the outstanding payments owed to a medical practice, healthcare organization, group, clinic, etc., for services rendered. Despite meticulous adherence to billing guidelines and a highly trained team, some claims inevitably face rejection or denial.
This is where the accounts receivable follow-up team steps in, tasked with reopening and securing rightful reimbursement for denied claims. Surprisingly, a significant portion of these claims, often resulting from simple errors, go unaddressed, leaving healthcare providers forfeiting thousands of dollars annually.
2. What are the consequences of poor AR management?
Poor AR management can cause disruptions in the cash flow essential for sustaining day-to-day operations. This delay in payments not only hampers the financial stability of the healthcare organization but also restricts its ability to potentially invest in critical areas that an improve the billing process, like training of team members.
Moreover, inadequate A/R management can lead to increased administrative burdens, as healthcare providers find themselves entangled in the complexities of claim denials, rejections, and subsequent follow-ups. This administrative overhead not only consumes valuable time and resources but can also compromise the overall quality of patient care.
Additionally, the interconnected nature of billing processes means that inefficiencies in A/R management could flow through the entire revenue cycle, timely claim submissions, and, ultimately, the reimbursement process.
3. What are the Benefits of Improving AR within Billing?
The advantages of optimizing the Accounts Receivable process extend beyond mere financial stability. Here’s a detailed exploration of the benefits:
- Reduced Delays in Payment: Streamlining AR follow-up ensures that payments are processed swiftly, minimizing delays and contributing to a consistent and predictable cash flow. Swift payment cycles enhance the financial health of a healthcare organization, providing resources for ongoing operations and investments.
- Enhanced Financial Health: A well-managed AR system directly correlates with improved financial health. Efficient revenue collection enables healthcare practices to meet financial obligations and pursue growth opportunities. Financial stability is foundational for healthcare organizations, allowing them to invest in technology, staff training, and infrastructure, ultimately enhancing the quality of patient care.
- Consistent, High-Quality Patient Care Services: An optimized AR process translates to more resources allocated for patient care services. This contributes to consistent, high-quality healthcare delivery. Adequate financial resources empower healthcare providers to invest in advanced medical technologies, ongoing staff training, and patient-focused initiatives.
- Operational Efficiency: Operational efficiency is a natural byproduct of an optimized AR process. Streamlined workflows and timely payments contribute to a well-functioning healthcare organization. Efficiency in operations not only reduces administrative burdens but also allows healthcare providers to allocate more time and resources to patient care.
4. How to Improve AR?
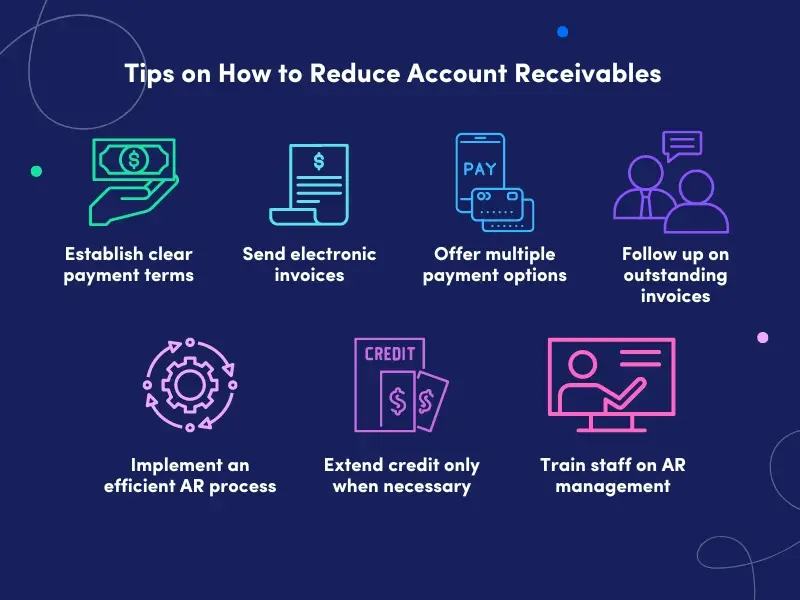
Delving into actionable strategies is key to enhancing Accounts Receivable within healthcare billing. Here’s a detailed roadmap for improvement:
- Addressing Denied Claims and Reopening Effectively: Analyze the reasons behind denied claims, implement corrective measures, and develop a systematic process for reopening claims to maximize reimbursement. Addressing denials promptly improves the likelihood of claim approval, preventing revenue loss and maintaining a healthy cash flow.
- Understanding the Significance of Accurate Diagnosis and Procedure Codes: Emphasize the importance of precise coding to avoid claim denials. Educate staff on the significance of accurate diagnosis and procedure codes. Accurate billing and coding is fundamental to the reimbursement process. It reduces the risk of denials, streamlining the entire AR process.
- Practical Steps to Optimize AR Processes: Implement practical measures such as staff training, technology integration, and continuous monitoring to optimize AR processes. Practical steps ensure a proactive approach to AR management, fostering continuous improvement and adaptability to evolving billing requirements.
5. How Outsourcing Medical Billing Can Improve the Financial Health of a Healthcare Organization
Outsourcing billing in the healthcare sector is gaining momentum as organizations recognize its value, offering expertise and opportunities for revenue improvement. This upward trajectory is expected to persist in 2024.
With over 12 years of experience, Neolytix guarantees enhanced cash flow, decreased administrative workload, and cost savings by optimizing the revenue cycle efficiently. Our comprehensive strategy, from ensuring compliance excellence to our proven track record, safeguards revenue and financial stability for healthcare organizations.
Contact us today to schedule a demo and discover how Neolytix’s expert medical billing assistance can reduce accounts receivable and propel your healthcare organization to thrive in 2024.