Negotiating contracts with payers is crucial for maintaining financial health, ensuring high-quality patient care and healthy business relationships. Effective payer contract negotiations can lead to better reimbursement rates, improved cash flow, and a more sustainable practice.
This article delves into proven strategies that healthcare organizations can use to enhance their payer contract negotiations.
Understanding the Importance of Payer Contract Negotiations
Securing favorable contracts with payers is crucial for any healthcare organization, significantly shaping the financial landscape and operational capabilities of a practice. Here are other key elements of effective payer contract negotiations:
- Critical for Financial Sustainability: Negotiating contracts with healthcare payers is essential for maintaining the financial health of medical organizations.
- Determines Reimbursement Rates: These contracts set the rates at which services are reimbursed, directly affecting the revenue cycle and cash flow.
- Ensures Fair Compensation: Effective negotiations help ensure that the practice receives compensation that accurately reflects the quality and cost of care provided.
Mastering payer contract negotiations not only supports immediate financial stability but also ensures a robust foundation for future growth and excellence in patient care.
Why Payer Contract Negotiations are Critical for Healthcare Organizations
Securing favorable contracts with payers is vital, but here are other reasons that highlight the importance of engaging in effective payer contract negotiations:
- Secure Better Reimbursement Rates: Engaging in payer contract negotiations allows healthcare organizations to obtain more favorable reimbursement rates.
- Avoid Financial Strain: Without effective negotiations, providers might be stuck with contracts that don’t adequately cover the cost of services, leading to financial difficulties.
- Support Financial Health: Negotiating favorable terms helps ensure fair payment for services, which in turn supports the organization’s financial stability.
- Invest in Patient Care Improvements: Adequate reimbursement rates enable providers to reinvest in their practice, enhancing the quality of care offered to patients.
Overview of Common Challenges Faced During the Negotiation Process
Negotiating with payers comes with several challenges. Providers often face resistance from payers who aim to minimize their reimbursement rates. The complexity of contract terms and the legal language used can also pose difficulties.
Additionally, providers must balance maintaining good relationships with payers while advocating for better terms. Navigating these challenges requires preparation, strategic planning, and a clear understanding of both parties’ needs.
Identifying and Negotiating Key Contract Clauses
Understanding and negotiating key contract clauses is crucial to ensuring fair terms and avoiding potential pitfalls. Here are some critical clauses to be aware of:
Clause | Description | Negotiation Strategy |
Hold Harmless | Protects one party from being held liable for certain risks. | Negotiate for mutual clauses that share liability equally, ensuring both parties are protected. |
Arbitration | Requires disputes to be resolved through arbitration rather than court. | Ensure the arbitration process is neutral by specifying the use of a professional arbitration organization. |
Parties, Roles and Responsibilities | Outlines the roles and responsibilities of each party in the contract. | Clarify and balance the responsibilities to prevent an undue burden on either party. |
Payment Terms | Details the payment schedule, rates, and methods. | Negotiate clear and favorable payment terms, including timelines for claim submissions and payments.
|
Service Coverage | Specifies the services covered under the contract. | Ensure comprehensive coverage that aligns with the services your practice offers.
|
Policy Change notifications | Requires notification of any changes in policy affecting the contract. | Include a clause that mandates advance notice of any policy changes, with an option to terminate the contract if needed. |
Contract Renewal | Defines the terms and conditions for renewing the contract | Negotiate favorable renewal terms, including clear renewal dates and the process for renewal discussions. |
These strategies help ensure that the contract terms are fair and beneficial, protecting both parties from future disputes and misunderstandings.
Importance of Preparing Well in Advance
Preparation is key to successful payer contract negotiations. Ideally, providers should start preparing at least 12 months before the contract renewal date. This preparation includes gathering data on current reimbursement rates, analyzing payer performance, and understanding market trends.
Early preparation allows providers to develop a strong negotiation strategy, identify potential areas for improvement, and avoid last-minute pressure that can lead to unfavorable terms.
Crafting a Data-Driven Argument to Demonstrate Value to Payers
In payer contract negotiations, data is a powerful tool. Providers and organizations can use data to demonstrate their value to payers, highlighting how their services contribute to better patient outcomes and cost savings. By presenting concrete evidence of their performance, providers can make a compelling case for higher reimbursement rates.
Tips on Using Quality and Cost Metrics to Support Your Case
- Patient Satisfaction Scores: Showcase high patient satisfaction ratings to highlight the quality of care.
- Clinical Outcomes: Present data on successful clinical outcomes, such as reduced hospital readmission rates.
- Cost-Efficiency Measures: Demonstrate cost savings achieved through efficient care delivery.
- Comparison to Industry Standards: Compare your performance metrics to industry benchmarks to further strengthen your case.
How to Highlight Your Practice’s Unique Strengths
By showcasing these strengths, providers can differentiate themselves from competitors and justify higher reimbursement rates.
- Remote Patient Monitoring: Highlight the benefits of remote patient monitoring, such as continuous care, early detection of health issues, and reduced hospital visits.
- Automation: Showcase how automation streamlines administrative tasks, improves accuracy, and frees up more time for patient care.
- Specialized Care Programs: Highlight unique offerings like behavioral health integration or chronic disease management programs.
- Added Value: Demonstrate the additional value these services bring to patient care, setting your practice apart from competitors. This differentiation helps in contract renewal negotiation and justifying higher reimbursement rates.
Key Negotiation Strategies
Understanding Both Sides’ Interests
- Mutual Benefits and Shared Goals: Emphasize the mutual benefits and shared goals of both parties. Both providers and payers aim to deliver high-quality, cost-effective care. By framing negotiations around these shared objectives, you can foster a collaborative atmosphere and work towards mutually beneficial outcomes.
Building and Maintaining Long-Term Relationships with Payers
Establishing and nurturing strong relationships with payers is key to successful contract negotiations. Here are strategies to build and maintain these crucial relationships:
- Regular Communication: Keep payers updated on positive developments and any changes or improvements in your practice, such as new services or enhanced patient care initiatives.
- Scheduled Meetings: Hold regular meetings to discuss performance metrics, contract terms, and address any concerns. This fosters open dialogue and helps resolve issues early.
- Quality Improvement Initiatives: Involve payers in quality improvement projects, demonstrating your commitment to high-quality care and collaboration.
- Collaborative Projects: Engage in joint initiatives like shared savings programs, which benefit both parties and strengthen partnerships.
- Addressing Concerns: Promptly address payer concerns to show your dedication to maintaining a strong, responsive relationship.
- Transparency: Be open about your practice’s performance and challenges. Honest communication builds trust and supportive payer relationships.
By consistently applying these strategies, healthcare providers can secure better contracts and build a foundation for ongoing success.
Comparing Payer Rates
- Analyze and Compare Rates: Conduct a thorough analysis of the reimbursement rates offered by different payers for the same services. This can highlight discrepancies and provide a basis for negotiating higher rates.
- Data-Driven Negotiations: Use de-identified data to compare payer performance and build a strong case for rate adjustments. For example, if Payer A reimburses $100 for a particular service while Payer B only reimburses $80, you can use this data to negotiate with Payer B for a higher rate, presenting the $100 reimbursement as a benchmark.
Tips on Negotiating for Higher Rates for High-Volume Services
- High-Volume Services: Focus on securing higher rates for high-volume services, such as office visits. This can significantly impact your revenue.
- Demonstrate Impact: Show how the volume of these services affects overall patient care to justify higher reimbursement rates.
Leveraging Value-Based Care Models
- Shift to Value-Based Care: The healthcare industry is moving towards value-based care models, which emphasize quality and outcomes over volume. This shift has significant implications for payer contract negotiations.
- Highlight Successes: Leverage your success in improving patient outcomes and reducing costs to negotiate better terms.
How Aligning Incentives Can Benefit Both Payers and Providers
- Mutually Beneficial Agreements: Aligning incentives between payers and providers can lead to mutually beneficial agreements.
- Shared Savings Programs: Propose shared savings programs or performance-based incentives that reward both parties for achieving specific healthcare outcomes.
- Demonstrate Value: Show how these arrangements can lead to cost savings and better patient care to negotiate more favorable terms.
Using Negotiation Checklists
A comprehensive negotiation checklist is an essential tool for successful payer contract negotiations. It ensures that no critical elements are overlooked and provides a structured approach to the negotiation process.
Key Items to Include in Your Checklist
- Payment Terms: Clearly defined payment rates, schedules, and methods.
- Service Coverage: Detailed list of services covered under the contract.
- Policy Change Notifications: Clause requiring advance notice of any policy changes.
- Contract Renewal Terms: Specific terms and conditions for contract renewal, including renewal date and clauses.
- Fee Schedules: Detailed fee schedules for all covered services.
- Renewal Clauses: Clear clauses regarding the contract renewal process and any required documentation.
- Expiration Dates: Clearly defined expiration dates for the contract and any associated agreements.
- Contract Terms: Detailed contractual terms that govern the agreement.
- Cost-Saving Provisions: Clauses that outline any cost-saving measures or incentives.
- Contract Periods: Defined periods for which the contract is valid, including any probationary periods.
By incorporating these items into your negotiation checklist, you can ensure a thorough and effective negotiation process, leading to more favorable contract terms.
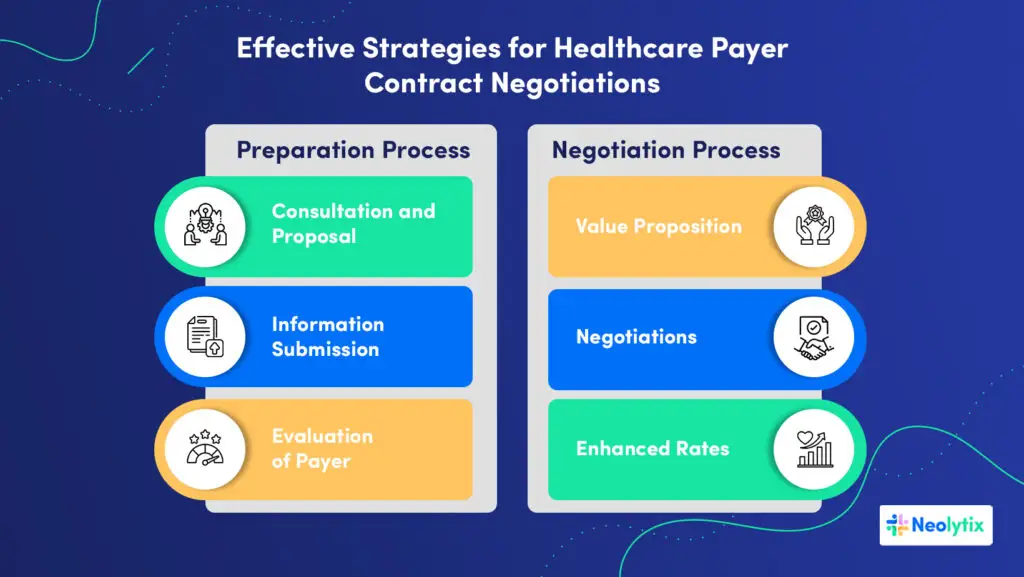
Effective Strategies for Healthcare Payer Contract Negotiations
Neolytix specializes in providing comprehensive healthcare payer contract management, guiding medical providers through an effective negotiation process through a rigorous:
Preparation Process
- Consultation and Proposal: Discuss your current contracts and needs. We then submit a proposal outlining the process, fees, and timelines.
- Information Submission: Provide us with the necessary data to analyze your rates and create a strong proposal.
- Evaluation of Payer Reimbursements: Compare your rates for each CPT code with Medicare’s rates to understand your financial performance.
Negotiation Process
- Value Proposition: Present a detailed offer highlighting your unique capabilities, cost-effectiveness, and quality of care.
- Negotiations: Submit the value proposition to each plan and begin the negotiation process, pushing for higher rates with strong evidence.
- Enhanced Rates: Persistently pursue negotiations until your practice attains the deserved rate increase.
Take Action with Neolytix
By partnering with Neolytix, you gain access to our proven strategies and 12 years of deep industry knowledge. We work closely with you to understand your unique challenges and goals, developing customized solutions that enhance your negotiation outcomes.
Our focus on mutual benefits, value-based care and long-term relationships ensures that you not only achieve favorable contract terms but also build a strong foundation for future negotiations.
Schedule a no-obligation consultation today to secure the future financial outlook of your healthcare organization.
Schedule A Free Consultation
"*" indicates required fields



