Chronic care management (CCM) has emerged as a vital strategy for healthcare providers seeking to enhance patient outcomes, increase revenue, and expand their patient base. By leveraging CCM services, healthcare providers can proactively address the complex needs of patients with chronic diseases, ensuring better care coordination, improved patient engagement, and optimized healthcare delivery.
In this article, we will explore topics such as what chronic care management is, its benefits for healthcare providers, the advantages of outsourcing this service to external providers, etc.
Table of Contents
What is Chronic Care Management (CCM)?
Chronic care management refers to the proactive, ongoing care provided to individuals with chronic diseases such as diabetes, heart disease, and COPD. These conditions often require comprehensive care plans, regular follow-ups, and effective coordination among healthcare professionals. CCM aims to optimize patient care by establishing a dedicated care team, promoting patient engagement, and leveraging technology for streamlined communication and data management.
Medicare began paying for CCM services separately under the Physician Fee Schedule (PFS) in 2015. For instance, healthcare providers can now request payment for Chronic Care Management (CCM) for a specific month if they dedicate a minimum of 20 minutes to non-face-to-face tasks related to coordinating care for Medicare patients with multiple chronic conditions. These activities, overseen by a physician or another qualified healthcare professional, aim to manage and organize the healthcare of eligible patients.
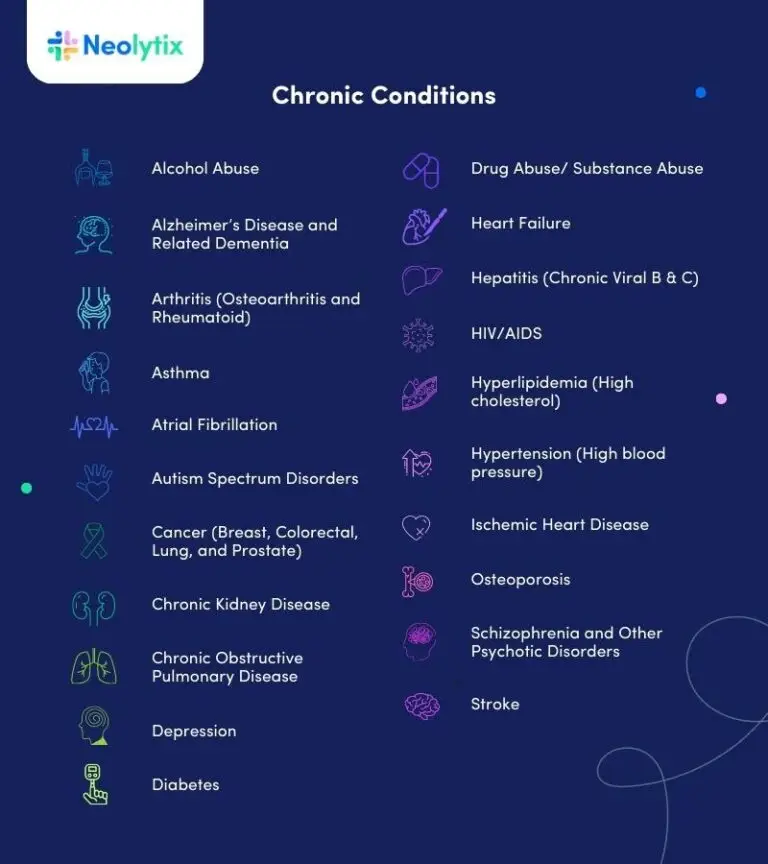
Below is a list of the conditions as stipulated by CMS:
Why should a Medical Provider Implement Chronic Care Management?
By implementing chronic care management, healthcare providers can significantly improve the quality of care for their patients but also create new revenue streams at their healthcare organization.
Improving Patient Care
CCM services include creating a comprehensive care plan tailored to each patient’s unique needs, regular communication and follow-up visits, medication management, and patient education.
At the start of 2015, chronic care management (CCM) was a relatively unfamiliar concept for physicians. However, by 2016, a significant amount of information regarding CCM became more widely available. This included compelling data that provided evidence supporting the program’s benefits. Testimonials showcasing the revenue generated, enhanced health outcomes, cost savings, and instances where CCM played a crucial role in saving lives became more prevalent. As a result, physicians became more engaged and subsequently adopted CCM in their practice.
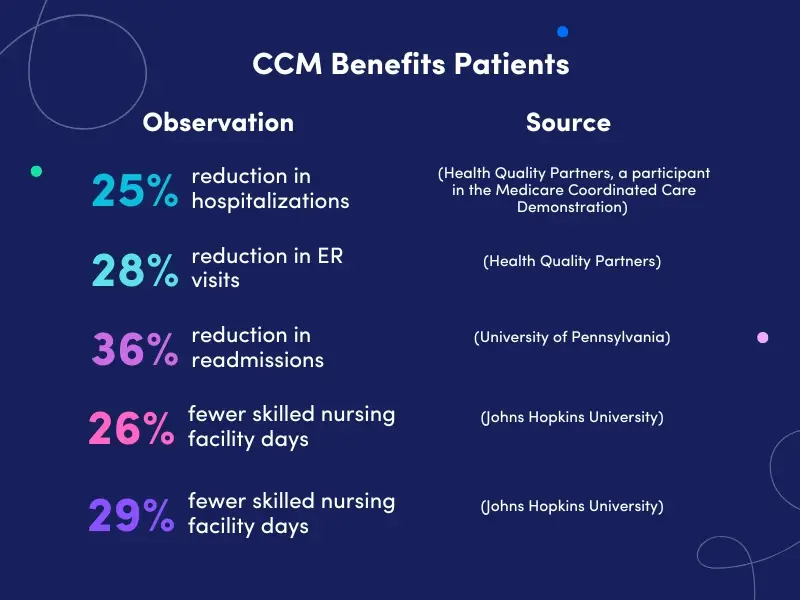
According to the various studies conducted to determine the efficacy of chronic care management and remote patient monitoring, patient care and health improvements became evident.
Boosting Revenue and Patient Base
Adopting chronic care management can have a positive impact on healthcare providers’ financial sustainability. The Centers for Medicare and Medicaid Services (CMS) recognize the value of CCM and have established CPT codes, such as the widely used code 99490, to reimburse providers for these services.
By offering CCM services, healthcare providers can increase their revenue by billing for the additional time and resources invested in managing chronic diseases. Moreover, providing comprehensive care for chronic conditions can lead to higher patient satisfaction, resulting in increased patient loyalty and referrals, consequently expanding the patient base.
Exploring Opportunities in Chronic Care Management: A Fresh Look at Best Practices and Strategies
The rise of chronic care management (CCM) has opened a significant pathway for healthcare organizations to enhance patient outcomes and streamline operations. While the concept may seem straightforward, optimizing processes and understanding the financial impact can turn CCM into a true asset for healthcare providers. Below, we explore key insights on how to start a chronic care management business, CCM guidelines, and steps to integrate this service seamlessly into your practice.
For healthcare organizations or independent providers looking to dive into CCM, the first step is understanding the chronic care management workflow. A successful CCM initiative requires a cohesive approach involving patient identification, creating comprehensive care plans, and maintaining continuous engagement through regular follow-ups. Providers should also ensure that they meet CCM care plan requirements, as outlined by Medicare and chronic care management CMS guidelines.
How to Start the Chronic Care Management Process?
The process of chronic care management involves several vital steps to ensure effective care coordination and improved patient outcomes. Here’s an overview of how the process typically works:
1. Identification of Eligible Patients
Healthcare providers identify patients with chronic diseases who would benefit from chronic care management services. These patients often have multiple chronic conditions and require ongoing care and support.
2. Development of a Comprehensive Care Plan
A dedicated care team consisting of physicians, nurses, and other healthcare professionals, creates a comprehensive care plan tailored to each patient’s needs. The plan includes goals, interventions, medication management, and patient education.
3. Regular Communication and Follow-Up
The care team conducts regular check-ins with patients, either in-person or via telehealth, to assess their health status, address concerns, and provide necessary support. Communication channels, such as secure messaging or phone calls, facilitate ongoing engagement between patients and their care team.
4. Medication Management
The care team monitors patients’ medication adherence, adjusts prescriptions as needed, and ensures proper medication management. This helps prevent adverse drug interactions and optimizes treatment effectiveness.
5. Patient Education and Self-Management
Patient education plays a vital role in empowering individuals to manage their chronic conditions actively. The care team provides resources, guidance, and support to help patients understand their conditions, make lifestyle modifications, and adhere to treatment plans.
Establishing a business model around CCM can open up multiple revenue streams while improving patient care. To get started, familiarize yourself with chronic care management billing practices and chronic care management CPT codes like 99490 and 99491, which offer structured reimbursement opportunities. Understanding these codes is essential for healthcare organizations aiming to improve financial sustainability while maintaining compliance with chronic care management guidelines.
Creating an Effective Chronic Care Management Workflow
At the core of a successful CCM program is an efficient workflow that ensures patients with chronic conditions receive timely, coordinated care. The ideal chronic care management workflow begins with identifying eligible patients, which typically involves those with multiple chronic conditions. Once identified, providers must create detailed chronic care management care plans that outline care strategies, medication management, and patient education.
These chronic care management care plan requirements are crucial for ensuring patients receive personalized care, which includes setting achievable health goals and offering continuous support. Additionally, chronic care management companies often utilize technology to track patient progress and monitor adherence to care plans, further enhancing outcomes.
CPT Codes for Chronic Care Management
Healthcare providers utilize specific Current Procedural Terminology (CPT) codes to bill for chronic care management services. The primary CPT code for chronic care management is 99490. This code covers at least 20 minutes of non-face-to-face care coordination and management services per calendar month. It includes services like care plan development, communication with other healthcare professionals involved in the patient’s care, medication management, and 24/7 access to care.
In addition to 99490, providers can use other CPT codes to bill for an extended time or more complex cases, such as 99487 (60 minutes) and 99489 (additional 30 minutes beyond the initial 20 minutes of 99490).
Chronic Care Management & Principal Care Management Codes
CPT Code
Descriptor (Summary)
99424
Principal care management services involve a single high-risk chronic condition lasting at least 3 months, with complex care needs, frequent medication adjustments, and coordination among practitioners. The first 30 minutes of care per month must be provided by a qualified healthcare professional.
99425
Additional principal care management services for a high-risk chronic condition lasting at least 3 months include complex care planning, medication adjustments, and ongoing coordination between practitioners. Each extra 30 minutes per month must be provided by a qualified healthcare professional.
99426
Initial principal care management services for a high-risk chronic condition lasting at least 3 months include complex care planning, medication adjustments, and ongoing coordination between practitioners. The first 30 minutes of clinical staff time per month must be directed by a qualified healthcare professional.
99427
Additional principal care management services for a high-risk chronic condition lasting at least 3 months include complex care planning, medication adjustments, and ongoing coordination between practitioners. Each extra 30 minutes of clinical staff time per month must be directed by a qualified healthcare professional.
99437
Additional chronic care management services for patients with multiple chronic conditions lasting at least 12 months include comprehensive care planning and monitoring. Each extra 30 minutes per month must be provided by a qualified healthcare professional.
99439
Chronic care management services, each additional 20 minutes of clinical staff time directed by a physician or other qualified health care professional, per calendar month
99487
Initial complex chronic care management services for patients with multiple chronic conditions lasting at least 12 months include comprehensive care planning and moderate or high-complexity medical decision-making. The first 60 minutes of clinical staff time per month must be directed by a qualified healthcare professional.
99489
Additional complex chronic care management services for patients with multiple chronic conditions lasting at least 12 months include comprehensive care planning and moderate or high-complexity medical decision-making. Each extra 30 minutes of clinical staff time per month must be directed by a qualified healthcare professional.
99490
Initial chronic care management services for patients with multiple chronic conditions lasting at least 12 months include comprehensive care planning. The first 20 minutes of clinical staff time per month must be directed by a qualified healthcare professional.
99491
Chronic care management services are provided by a qualified healthcare professional for patients with multiple chronic conditions lasting at least 12 months. Requires a comprehensive care plan and at least 30 minutes of professional time per month.
Understanding the Value of Chronic Care Management Reimbursement
One of the significant benefits of offering CCM services is the potential to generate additional revenue by CCM reimbursement. Practices can utilize CCM CPT codes such as 99490 and 99491 to bill for non-face-to-face services, helping to compensate for the additional work involved in managing patients with chronic conditions. These CCM CPT codes have been a critical part of Medicare’s strategy to enhance chronic disease management while promoting preventive care.
For providers handling more complex cases, complex chronic care management codes such as 99487 allow for additional billing opportunities based on the complexity of care provided. Understanding CCM billing and how to maximize chronic care management reimbursement is essential for healthcare organizations looking to create a sustainable business model while improving care.
Additionally, healthcare practices focusing on single chronic conditions can explore principal care management billing guidelines, ensuring they bill appropriately for these services. Staying up to date with chronic care management CMS guidelines ensures your practice adheres to regulatory requirements, minimizing the risk of denied claims.
The process can be streamlined by outsourcing CCM to trusted chronic care management companies that specialize in managing these programs. Such companies are skilled in crafting effective chronic care management care plans, ensuring compliance, and handling chronic care management billing. This enables healthcare organizations to focus on delivering quality care while efficiently managing chronic disease populations.
Payers offering Chronic Care Management (CCM) Reimbursement
Several payers, including Medicare and some commercial insurers, offer reimbursement for chronic care management services. Medicare, through its Medicare Part B program, covers chronic care management for eligible beneficiaries.
Many commercial insurers have followed suit, recognizing the value of proactive chronic disease management. Healthcare providers must check with specific payers to determine coverage and reimbursement policies. Here are a few examples of commercial payers:
UnitedHealthcare is one of the largest commercial insurers in the United States and offers coverage for chronic care management services. They recognize the value of CCM in improving patient outcomes and reducing healthcare costs.
Aetna, now a part of CVS Health, provides coverage for CCM services. They emphasize the importance of proactive management of chronic conditions and offer reimbursement for eligible services.
Cigna is another prominent commercial payer that recognizes the value of chronic care management. They offer coverage for CCM services and work closely with healthcare providers to enhance care coordination and patient outcomes.
Various regional and state-based Blue Cross Blue Shield (BCBS) plans across the country provide coverage for chronic care management. Each BCBS plan may have specific guidelines and requirements, so checking with the local plan for coverage details is essential.
Humana is a leading healthcare company that offers coverage for chronic care management services. They focus on improving care coordination and patient engagement to achieve better health outcomes for individuals with chronic diseases.
The Advantages of Outsourcing Chronic Care Management
Outsourcing chronic care management services to external providers, like Neolytix, offers several benefits for healthcare organizations. By partnering with Neolytix, healthcare organizations can optimize their resources and focus on core areas of expertise. Here are some advantages of outsourcing chronic care management:
Expertise and Specialization
Neolytix has dedicated teams of specialists, including registered nurses and other healthcare experts experienced in chronic care management. They possess the necessary knowledge and skills to deliver high-quality care and navigate the complexities of CCM, allowing healthcare organizations to make the switch with minimal hassles.
Cost-effectiveness
Outsourcing CCM services eliminates the need for hiring and training additional staff, thereby reducing overhead costs. The extra time and money spent on training staff and the costs associated with a learning curve when adopting a new service are eliminated.
Neolytix customizes its service offerings and offers a pay-per-service model, allowing healthcare organizations to scale their CCM efforts based on patient volume and demand.
Technology and Infrastructure
Neolytix CCM teams leverage advanced technology and systems for efficient care coordination, patient engagement, and data management. By partnering with us, healthcare organizations can access these technological advancements without significant upfront investments.
Compliance and Regulatory Expertise
The ever-changing healthcare landscape requires adherence to various regulations and guidelines. Outsourcing CCM services to external service providers like Neolytix ensures compliance with billing, documentation, and reporting requirements, reducing the risk of penalties and audits.
Scalability and Flexibility
External CCM service providers like Neolytix offer scalable solutions to accommodate the fluctuating patient volume and evolving care needs. Healthcare organizations can quickly expand or contract their CCM services based on demand, ensuring optimal resource allocation.
How Chronic Care Management Vendors Support Your Practice
Working with trusted chronic care management vendors can make a significant difference in the effectiveness of your program. These vendors not only offer billing support but also assist with chronic care management technology that improves workflow and enhances patient communication. They also provide resources to help healthcare providers meet chronic care management documentation requirements, which is vital for ensuring compliance and securing CCM reimbursement.
Partnering with a chronic care management company that understands the nuances of chronic care management patient information and CCM healthcare management can simplify the entire process. These companies also help ensure that patient data is handled securely while maintaining compliance with HIPAA regulations, offering peace of mind for both providers and patients.
The Benefits of Chronic Care Management for Providers
Remember, the benefits of chronic care management extend beyond improving patient outcomes. By managing chronic conditions through proactive care, providers can reduce hospital readmissions, improve patient satisfaction, and foster long-term relationships with patients. These efforts are backed by Medicare’s emphasis on preventive care, offering chronic care management reimbursement opportunities that reward practices for their time and resources.
Meeting CCM Guidelines and Care Plan Requirements
Compliance with chronic care management guidelines is critical for providers to offer the best care while maintaining financial health. Providers must meet specific chronic care management care plan requirements to qualify for reimbursement. These requirements include developing a comprehensive care plan, documenting care coordination efforts, and maintaining regular communication with patients.
Chronic Care Management Providers: Building a Foundation for Success
Choosing the right chronic care management providers can greatly influence the success of your CCM program. These providers are often the backbone of effective care coordination, driving patient engagement and fostering long-term health improvements. For instance, providers must ensure that the care team follows established chronic care management guidelines to offer the best possible outcomes for patients. This approach is particularly effective when healthcare organizations invest in training their teams on chronic care management examples to illustrate the positive impacts of proper care planning.
Maximizing Efficiency with Chronic Care Management Solutions
For healthcare providers, chronic care management solutions offer a structured way to improve patient care while increasing operational efficiency. Whether you’re a small practice or a larger organization, implementing a well-managed chronic care system can help you provide better care for patients with long-term health conditions. By partnering with a reliable chronic care management company, healthcare providers can offload administrative tasks while maintaining direct oversight of care delivery. This collaboration streamlines the process, allowing your team to focus on higher-priority patient care while ensuring compliance with chronic care management documentation requirements.
Streamlining Care with Chronic Care Management Service Companies
Outsourcing your chronic care needs to chronic care management service companies can provide several immediate benefits. These companies bring in expertise to manage CCM billing, chronic care management patient information, and day-to-day communication with patients. These services alleviate the administrative burden on your in-house staff, offering them more time to focus on direct patient care. Furthermore, outsourcing helps ensure adherence to chronic care management codes and Medicare’s guidelines, especially for Medicare chronic care management billing.
These service providers also specialize in using chronic care management technology to help manage communication, monitor patient progress, and store vital data efficiently. The use of such technology can streamline operations and make it easier to implement CCM chronic care management programs that deliver both high-quality care and higher reimbursements.
Summary
Chronic care management presents a valuable opportunity for healthcare providers to enhance care, increase revenue, and grow their patient base. By implementing CCM services and leveraging the expertise of dedicated care teams, healthcare organizations can provide comprehensive, coordinated care for patients with chronic diseases.
Additionally, outsourcing chronic care management to external service providers offers numerous advantages, including specialized expertise, cost-effectiveness, access to advanced technology, and compliance support. Embracing chronic care management is a proactive step towards improving patient outcomes and positioning healthcare providers for success in a value-based care environment.
Neolytix offers remote patient monitoring and chronic care management to help healthcare organizations unlock revenue streams from their existing patient base and improve patient care, without having to go through an extensive learning curve or put additional strain on their resources.
Schedule a no-obligation consultation to learn more or request a quote straight away.
Complete the form and someone from our team will be in touch with you!



