Turn Provider Credentialing from a 90-Day Marathon into a 45-Day Sprint
Incredibly combines intelligent automation with secure workflows to cut your enrollment time in half—while keeping your compliance team happy and your providers productive.
Every Day a Provider Waits = Lost Revenue
You know the drill: New provider hired. Excitement high. Then… crickets for 90-120 days while credentialing crawls along. Meanwhile, that provider is costing you money instead of making it.
What if credentialing could be as smooth as your clinical operations?

Meet Incredibly: Your Automated Credentialing Assistant
Think of Incredibly as your organization’s most efficient credentialing specialist—one who never sleeps, never loses a document, and never forgets a deadline. Built by healthcare operations experts who’ve walked in your shoes, it’s the solution that finally makes provider enrollment… manageable.
How Incredibly Transforms Your Workflow:
Built for Real Healthcare Operations
For CFOs Looking at the Bottom Line:
- Let’s talk ROI. A single provider waiting 90 days to start seeing patients could mean $120,000 in lost revenue. Incredibly typically cuts that wait time in half.
- 45-60 day average credentialing time (vs. industry standard of 90-120 days)
- 80% reduction in manual data entry through intelligent automation
- No technology implementation costs—it’s already built and ready to go
For Operations Leaders Who Need Results:
- Complete visibility into every application’s status
- Proactive expiration alerts before credentials lapse
- Seamless EMR integration with major systems
- Dedicated Neolytix team backing up the technology

The Neolytix Difference:

250+ healthcare organizations
trust us with their operations

13 Years
Years of Combined Industry Experience

Global team of experts
supporting you

Continuous platform improvements
based on real user feedback
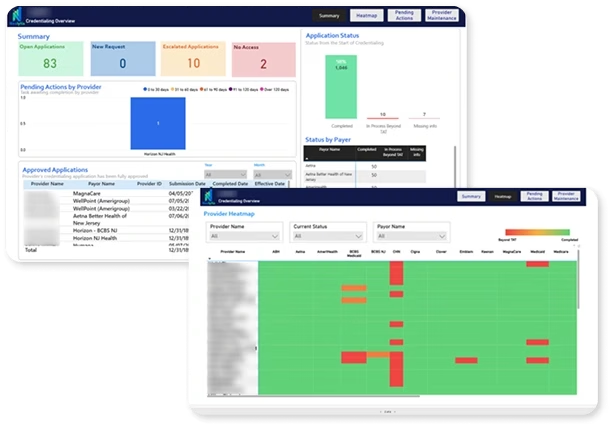
See Your Future Credentialing Workflow
Check Your Dashboard
Log in to see a clean, visual overview of all pending actions. No more spreadsheet hunting or email archaeology.

Automated Updates Run
While you focus on strategic work, Incredibly sends reminders, collects documents, and updates statuses automatically.

Review and Approve
Our team reviews completed applications with all supporting documents organized and ready. One click to submit.

Sleep Well
Know that expiration alerts are set, compliance is tracked, and nothing will fall through the cracks.

It's Time to Work Smarter, Not Harder
Your credentialing team is talented. But they’re drowning in paperwork, chasing documents, and managing spreadsheets.
Incredibly frees them to do what humans do best: solve problems, build relationships, and drive strategy.
The technology handles the repetitive stuff:
- Document collection and organization
- Action Prioritization
- Status tracking and updates
- Reminder sequences
- Compliance monitoring
- Report generation
Schedule Your Personalized Demo
Medical Credentialing Quote (Active)
"*" indicates required fields
Ready to Cut Your Credentialing Time in Half?
Let’s show you exactly how Incredibly can transform your provider enrollment process.